Some Hungarian hospitals have been facing a serious infection situation for years. Yet nothing happens to them
After Direkt36 with the help of the Hungarian Civil Liberties Union obtained and analyzed official data on hospital-acquired infections in Hungary between 2017 and 2022, a more detailed picture was revealed of the situation than ever before. The authorities responsible for public health have kept this information secret for a long time, but after a long litigation process, they have finally released it, giving us an insight into how many and what types of infections are being reported by inpatient care facilities in Hungary.
The database contains information on three types of infections that hospitals are obliged to report to the National Centre for Public Health and Pharmacy (NCPHP). These are infections that can cause serious complications or even death in hospital patients, especially if they are in a weakened condition.
Never before has such recent and extensive data on this subject been published in Hungary. The main findings of the analysis of this data are the following:
- Some hospitals have consistently high infection rates year after year compared to others. The hospitals that have had high incidences of at least two types of infections in almost every year since 2017 were analyzed in more detail. These were the Bajcsy-Zsilinszky Hospital in Kőbánya, Honvéd Hospital, Jahn Ferenc Hospital, the National Institute of Oncology (Országos Onkológiai Intézet – OOI) and Toldy Ferenc Hospital in Cegléd.
- There have been few changes at the top of the list compared to our analysis based on 2015-2016 data, indicating that despite the institutions reporting the data, health authorities are either inactive or their efforts are ineffective.
- The year after the outbreak of the coronavirus epidemic, 2021, had the highest infection rates according to the figures, and although the following year saw a slight decrease in the incidence of hospital-acquired infections, hospitals still reported almost double the number of infections of all three types of infection compared to 2017.
- One hospital’s data shows that the incidence of bloodstream infections in the neurology unit has increased sevenfold in six years, and in another institution, the incidence of all three infection types has at least doubled in the cardiology unit.
- According to the data the majority of infected patients in one hospital’s unit did not survive their hospital stay in 2022. However, this does not mean that the infection caused their death, as hospitals only report a link between the infection and cause of death in a fraction of cases.
This article is a follow-up to Direkt36’s series of articles called Semmelweis Project launched last autumn, in which we showed that the government is aware of the serious problem of hospital-acquired infections (or nosocomial infections), but is trying to hide it from the public. In our previous articles, we used data from 2015-2016 to rank how hospitals are performing compared to each other in terms of hospital-acquired infections, but we have since received data for 2017-2022.
Help us tell the truth in Hungary. Become a supporter!
While the database obtained by Direkt36 contains more detailed information on hospital-acquired infections than ever before, it does not show the complete picture. It only includes infections that are reported by hospitals to the NCPHP.
However, this institution and other authorities recognize that the reporting discipline of hospitals is loose.
The database also reveals that some active inpatient facilities have not reported any infections in six years, but there is little chance that there have been no infections at all. András Csilek, an infectologist and chairman of the Hungarian Medical Chamber’s Borsod-Abaúj-Zemplén county organisation, told Direkt36 that there are always nosocomial (hospital-acquired) infections in active inpatient units such as internal medicine, surgery, pulmonology and urology, and if they report that they have not had any, that is certainly not correct in his opinion.
We tried to get a response to the results of our analysis and the questions raised from all the hospitals concerned, as well as from the authorities responsible for public health. The majority of hospitals did not respond, and the NCPHP wrote this despite the fact that the hospital rankings we shared with them were developed with a nationally recognised biostatistician who used methods to filter out factors that could distort the comparison.
Those infections are called hospital-acquired infections, which develop during the process of receiving healthcare. András Csilek tried to give Direkt36 a nuanced picture. He told us that the bacteria that later become pathogens are often already present in patients when they are admitted, but have not previously made them ill, while weakened immune systems and invasive procedures increase the chances of infection.
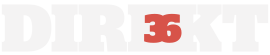
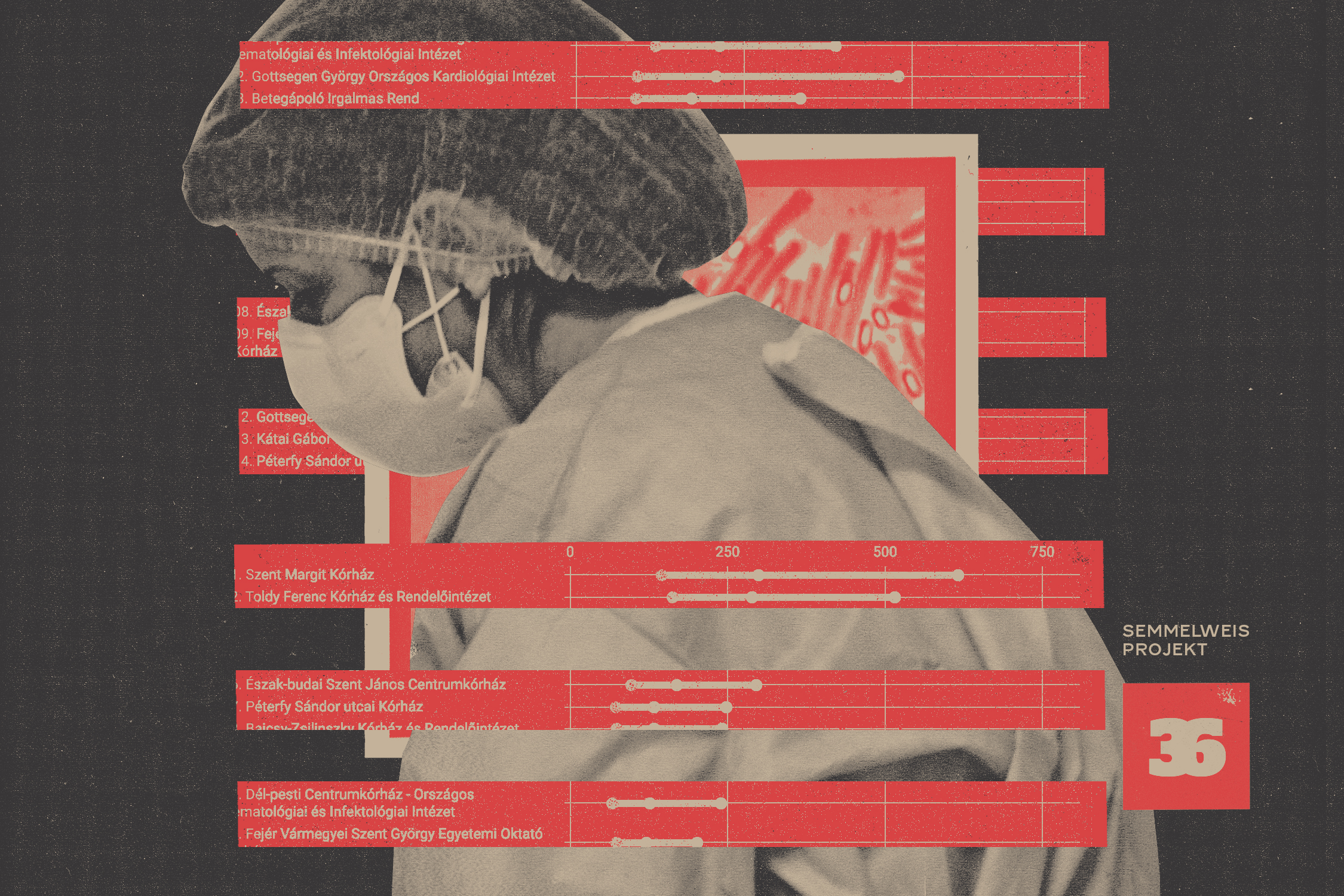
The annual rankings of hospital-acquired infections
Below you can see the rankings of Hungarian hospitals by different hospital-acquired infections. At the top of the charts are the hospitals with the highest incidence rates, and at the bottom are the hospitals with the lowest. The rankings are based on hospital-acquired infection data from 2017-2022. Our analysis of data from previous years, 2015 and 2016, can be found here.
The „Incidence” column shows the number of infections per 100,000 patient days. To make the rankings, we used statistical methods to reduce distortions caused by the different sizes of hospitals, the different types of hospital units, and patient groups. You can also filter by location and hospital name in the search box. By clicking on the years under the heading “data for other years”, you can access the rankings of hospitals for that particular year.
Those who want to know a more detailed explanation about the statistical modelling used to produce the rankings can find out more here. On the link you can also find out how we have filtered out from the list the institutions that have reported hospital-acquired infections to the authorities, but the statistical model cannot determine the ranking of them due to the limited data available.
On the first chart, hospitals are ranked by the prevalence of infections caused by multidrug-resistant pathogens that are resistant to many antibiotics. Multidrug-resistant pathogens are bacteria that can cause serious pneumonia, wound infections, urinary tract infections or even sepsis, especially among elderly or already sick patients.
The second chart shows which hospitals have had the highest incidence of clostridium difficile (CDI) over the years, a bacterial infection that causes severe diarrhea and dehydration and can even lead to life-threatening inflammation of the intestines.
The last table shows the rankings by incidence of bloodstream infections. Bloodstream infections occur when a pathogen enters the blood and then spreads to other organs which can be infected and shut down. It causes death in a significant number of cases.
If you want to see how infections have developed in the different hospital units in a given year, you can download the figures here and the graphs here. The original data given by the NCPHP can be downloaded from the links at the bottom of this article.
To analyze the data, we asked again Tamás Ferenci, one of the country’s most respected biostatisticians, for help. To reduce distortion due to differences in the mix of patients treated in different hospitals, he again used the same tried and tested method as he did with the 2015-16 data. For better comparability, he performed the analysis at the unit level instead of treating hospitals as a whole, and then made statistical corrections, but separately for each year.
There were no difficulties in creating yearly rankings, but it turned out that the possibilities for comparing individual hospitals and how their units changed over the long term were limited. The problem of the variation of patient mix is not only between different hospitals in the same year, but also between different years of the same hospital: new procedures may be introduced, possibly with a higher risk of infection, and patient characteristics (age, co-morbidities) may change over the years. Differences in the patient mix have been detected by using the so-called Cost Per Weighted Case numbers (that show how much funding a hospital receives for a patient and thus measures, the severity and complexity of the case). However, this solution only works for analyses of a given year. These figures are not constant: the National Health Insurance Fund recalculates them from time to time, so they cannot be used for long-term analysis. This means that comparisons between hospitals can only be made within a given year, and comparisons between different years are limited.
However, five hospitals have been at the top of at least two infection types in almost every year since 2017.
We investigated these hospitals – several of which were already featured in Direkt36’s series of articles last year – and took a closer look at which units have had the biggest increase in the incidence of hospital-acquired infections.
Watch Direkt36’s documentary on hospital-acquired infections with english subtitles!
A serious problem in Cegléd
The charts above show that certain hospitals are consistently at the top of the hospital-acquired infection rankings. One such example is the Toldy Ferenc Hospital in Cegléd, which has been among the worst performers in all infection types almost every year, meaning that it had high infection rates in the past six years.
Toldy Ferenc’s internal medicine unit experienced an increase in the incidence of all three infection types between 2017 and 2022: the incidence of clostridium difficile and bloodstream infections more than doubled, infections caused by multidrug-resistant pathogens increased more than one and a half times. The surgery units’ incidence of infections caused by multidrug-resistant pathogens almost doubled in six years.
Cardiology proved to be the most problematic unit, as our analysis showed a dramatic increase in the prevalence of all three types of infections with CDI more than three and a half times, multidrug-resistant pathogens almost three times, and bloodstream infections were twice as common in 2022 than in 2017.
According to the data between 2017 and 2022, 2026 hospital-acquired infections were reported, of which in 801 cases the patient did not survive the hospital stay. According to the NCPHP, since infections can overlap – meaning that a patient may have been infected with more than one pathogen – the actual number of patients who contracted infections and the number of deaths may be lower.
We wrote about Toldy Ferenc Hospital in our article last year, after the highest incidence of infections caused by multidrug-resistant pathogens had occurred there in 2015-16. The hospital’s management was aware of the shortcomings years ago, and published a pessimistic report setting out their strategy for 2018-2023. They mainly complained about the outdated infrastructure and the staff shortage, and acknowledged that the hospital had problems in reducing infections.
From our analysis, it seems that whatever was included in the strategy, there is still no solution to the conditions at the Toldy Hospital, which still had the highest incidence of multidrug-resistant infections in 2022. Dr. Ágnes Galgóczi, Head of the Hospital Hygiene and Public Health Department of the NCPHP admitted to Direkt36 in August 2023 that they were aware of the infection data of the Toldy Ferenc Hospital. According to her, however, it is not the responsibility of the NCPHP, but of the maintainer and management of the hospital to solve the problem. Direkt36 sent detailed questions to the National Hospital Directorate General, which funds the state hospitals, and to Toldy Ferenc Hospital, but none of the institutions responded to our request.
Help us tell the truth in Hungary. Become a supporter!
On top of the charts for years
Like Toldy Ferenc Hospital, Jahn Ferenc Dél-pesti Hospital has consistently been among the most problematic hospitals for several types of infections in almost every year that we examined.
Although the prevalence of infections has been somewhat reduced in the internal medicine unit which has a higher risk of infections, several units have reported a multiple increase in hospital-acquired infections. The incidence of bloodstream infections in the intensive care unit, which is also considered riskier in terms of infections, almost tripled in six years to 2022.
In the psychiatric unit of Jahn Ferenc hospital-acquired infections have been rising year after year,
even though this department does not typically perform surgery or serious invasive procedures – a medical procedure that invades (enters) the body, usually by cutting or puncturing the skin or by inserting instruments into the body – but at most injections, infusions or catheters. However, 11 cases of infection were recorded in 2022, 8 of which ended with death.
According to infectologist András Csilek, there are no more infectious patients in psychiatric units than elsewhere. If there are many infections reported, it is probably due to a “technical” reason, someone filled the spreadsheet wrongly and nobody noticed. He said it is possible that because many people are admitted to psychiatric wards with poor hygienic conditions, often homeless people straight from the street, who cannot be transferred to another ward because of their mental state, can infect the whole department.
The Jahn Ferenc Hospital did not report that the death of any psychiatric patient was linked to the infection. They registered that no connection between the death and the infection was found, or the connection was “unknown”.
In the neurology unit, the number of infections caused by multidrug-resistant pathogens has increased four times and the number of bloodstream infections has doubled. 1436 infected patients have died in the hospital in 6 years and 274 cases of infection were recorded as possibly being related to patient death.
The conditions at the Jahn Ferenc hospital were described in our previous article, as it was the hospital where no one noticed a dead body lying in the toilet for days in 2016. The cleaning company they had been working with was dismissed, but two years later they were hired again because they were 60 percent cheaper than the other tenderers.
In addition to infrastructural problems, according to its report the hospital is also facing a shortage of staff with 332 posts vacant in 2022, rising to 447 in 2023.
Debt and infections at the Honvéd Hospital
Another large hospital in Budapest, the Honvéd Hospital, has not managed to reduce hospital-acquired infections over the years. Between 2017 and 2022, the incidence of all three types of hospital-acquired infections increased in almost every department performing invasive procedures, including intensive care, internal medicine and surgery, which are particularly high-risk in terms of infections.
Neurology was one of their most critical departments, with CDI incidence tripling, prevalence of infections caused by multidrug-resistant pathogens increasing three and a half times, and bloodstream infections being seven times more common in 2022 compared to 2017 data.
Urology and cardiology also saw a rise in the incidence of all three infections.
Between 2017 and 2022, there were 1,841 reported cases of deaths of patients who had contracted a hospital-acquired infection at the Honvéd Hospital. The institution found a link between the patient’s death and the infection in 19 cases.
In 2019, a letter from a doctor working in the emergency care center described the conditions of his department as unacceptable and dangerous. According to the doctor, there was not enough equipment, staff were not paid overtime and, due to a lack of specialists, staff from other departments who had no experience in emergency care were transferred to their unit.
The problem was acknowledged by Béla Burányi, the head of the emergency care center at that time, who called the department dysfunctional. The interesting aspect of the case is that the NCPHP carried out an on-site inspection in the emergency care center of Honvéd Hospital a few months before the scandal broke and found everything in order.
Also in 2019, bedbugs covered the beds of on-call staff. Because the head of the department did not take the problem seriously at first, the staff had to live with the situation for weeks until the resting places of doctors and nurses in several on-call rooms became unusable.
The Honvéd Hospital did not respond to Direkt36’s request for comment.
Mice and infected people in Bajcsy hospital
The Bajcsy-Zsilinszky Hospital in Kőbánya has problems with hospital-acquired infections, according to our analysis. Between 2017 and 2022, 2892 hospital-acquired infections were recorded, and in 1366 cases patients with infections were reported (one patient can have several infections) to die in the hospital. According to their registrations, 361 death cases were linked to hospital-acquired infections. This figure is remarkable because it is much higher than elsewhere.
While, for example, in the Honvéd Hospital an average of one in 100 infected patients who died was found to have a connection between the infection and the patient’s death, the same conclusion was reached in a quarter of cases at Bajcsy.
András Csilek told Direkt36 that it is impossible that there is a difference of twenty-five times between the data of the two hospitals. At the same time, he said, it is not necessarily a manipulation of the reports, because the two hospitals may use different criteria to establish a link between infection and death. The infectologist said that the problem is rather that it is not at all certain that anyone in the authority has noticed the glaring difference or has thought about how to establish and implement a standardised methodology.
“If the journalist sees the difference, the authority probably sees it too, it just doesn’t address it. Or they don’t have the resources and the data goes to waste,” said Csilek.
At the Bajcsy-Zsilinszky Hospital, hospital-acquired infections were most problematic in surgery, internal medicine, infectology and intensive care units. There have been some very critical periods, for example, in 2021, 14 CDI cases and 56 bloodstream infections were recorded in the ICU from the beginning of February to the end of April.
In January 2019, Bajcsy appeared in the news when an outbreak of diarrheal disease forced the closure of several wards. In November 2019, a mouse was filmed in one of the paid rooms. In May 2020, there was a scandal when two nurses cared for patients with coronavirus with their faces uncovered because they had difficulty breathing under their masks. At that time, 24 staff members were infected. The hospital had such an abnormally high mortality rate during the coronavirus outbreak (one in three patients reportedly died) that the opposition party MSZP tried to clarify the situation in parliament, but the absence of government MPs resulted in the Public Welfare Committee meeting being inconclusive.
A surprise: National Institute of Oncology
The National Institute of Oncology (OOI) in Ráth Görgy Street, Budapest, is one of the best-equipped specialized hospitals in the country, with better-maintained buildings and infrastructure than the Toldy Hospital in Cegléd, which has been ranked at the top of our hospital-acquired infections lists for years.
From 2017 to the end of 2022, 822 hospital-acquired infections were reported in the National Institute of Oncology, of which 199 ended in death. Of these,108 cases (meaning every second case) were reported to be linked to a hospital-acquired infection.
The OOI management, when contacted by Direkt36, said that they considered it unprofessional to compare the infection data of serious cancer patients treated at the OOI with patients in other hospitals. The OOI wrote this even though, as we pointed out in our correspondence, Direkt36 was analyzing data at the unit level, comparing oncology only with other oncology departments, and even within that department, we were trying to reduce differences in patient mix.
The OOI also stressed in its response that their institution “provides the highest level of intensive care due to the radical cancer surgery and the lung transplant program, including ECMO”, which is an invasive procedure with a particularly high risk of infection.
The OOI also highlighted in its response that their institution “provides the highest level of intensive care due to the radical cancer surgery and the lung transplant program, including ECMO”, which is an invasive procedure with a particularly high risk of infection.
In its response, the National Institute of Oncology also pointed out that other hospitals are less thorough in detecting cases of infection and less disciplined in reporting data. In its reply to Direkt36, the institute included a table showing how many cases of each type of infection were reported between 2017 and 2021. However, in almost all cases, the figures differed from those in the NCPHP’s large database, which are also supposed to be reported by the OOI (there were some positive and some negative differences). We asked the NCPHP what the reason for this might be, but they did not answer our question.
The authorities’ data still does not seem reliable
The database obtained by Direkt36 also revealed several shortcomings of the reporting system. Hospitals reporting infections often leave certain fields blank. One example is whether the patient was isolated after being diagnosed with an infection caused by multidrug-resistant pathogens. In addition to yes and no, the options also include unknown, but in Toldy Ferenc hospital, for example, this field was left blank in 87 cases in 2021.
For patients with CDI, it is not revealed whether they have been isolated or not because no column in the database would answer to this.
András Csilek infectologist told Direkt36 that the oddities in hospitals reporting on the isolation of infected patients may be due to hospitals’ reluctance to admit that they are sometimes unable to comply with strict rules. Often there are not enough empty rooms or beds and it is physically impossible to move infected patients, and the hygienists who write the reports are not completely honest. “I can understand them in a way,” says Csilek, “who would like to make the situation look bad?”
Help us tell the truth in Hungary. Become a supporter!
Hospitals also very rarely register that the infection was linked to the patient’s death. In 2022, for example, the NCPHP reported that 34-42 percent of patients who contracted an infection did not return home, but hospitals only linked the infection to the patient’s death in 4-6 percent of cases.
The NCPHP itself recognizes that hospitals that report infections as required by the law look worse than those that fail to register cases. As we reported in our article last year, during the lawsuit filed for the latest data on hospital-acquired infections, it was argued that “low infection rates may be the result of insufficient infection identification rates (…) for example (e.g. very few blood samples are taken by doctors, so that a low number of bloodstream infections are laboratory-confirmed, which is required for reporting) or loose reporting discipline.”
Ildikó Remetehegyi, a specialist officer of the National Directorate General of Hospitals, who herself has experience as a hospital hygienist, gave a skeptical assessment of the NCPHP’s annual reports on hospital-acquired infections at a conference on infection control and patient safety last autumn.
“The data in the annual report are not valid, so the analyses based on them are flawed, and the strategies based on them are therefore ineffective,” she said. She said institutions manipulate their numbers to make the data “look pretty” and poor data quality does not allow progress to be made in the field. She also pointed out that fourteen percent of hospitals do not report hospital-acquired infections at all, and some submit that they had zero infection.
András Csilek said that nosocomial infections always occur in the inpatient departments of internal medicine, surgery, pulmonology and intensive care. However, among the institutions that have not reported any infections in the last six years is the Farkasgyepű Institute for Pulmonology, which has three pulmonology departments.
Direkt36 asked the institute how it was possible that they had not had any infections in six years, but they did not reply.
NCPHP: Thorough work, but misleading
György Surján, the NCPHP’s director of infection prevention and epidemiology, admitted at a press conference in November that Direkt36 had done a mathematically thorough job with the hospital infection rankings, but also called them “misleading”. He said that he was sorry that we had not approached them for help, because the NCPHP is willing to work with any expert on hospital infection data. “As far as the request is concerned, I was talking about a request from experts, not a request from the press”, he replied when we contacted him regarding this article.
Direkt36 has asked the NCPHP for help on several occasions in the past, we interviewed one of their staff, and we sent them a detailed series of questions before the publication of our “Semmelweis Project” article, to which they did not respond.
Direkt36 was not invited to the press conference in November, but encouraged by his statement, we emailed György Surján after obtaining new data. We sent him the methodology of the statistics we use and asked for his help to make our analyses more accurate. However, the director was not open to cooperation.
The original databases of hospital-acquired infections reported by institutions, which Direkt36 obtained with the help of the HCLU from the NCPHP, can be downloaded from the links below:
– Clostridium difficile infections – 2017, 2018, 2019, 2020, 2021, 2022
– Infections caused by multi-resistant pathogens – 2017, 2018, 2019, 2020, 2021, 2022
– Bloodstream infections – 2017, 2018, 2019, 2020, 2021, 2022
Cover photo by Péter Somogyi (szarvas) / Telex